
A Danish Diabetes Academy-funded postdoc project by researcher Rasmus Wibaek and colleagues recently published in Diabetologia gains special attention. The study used data from as far back as 1939 to examine the association between birth weight and risk of type 2 diabetes.
For every kilogram added to the birth weight of a child, the risk of developing type 2 diabetes is reduced by 40 percent. This is one of the findings of the Danish study Low birthweight is associated with a higher incidence of type 2 diabetes over two decades independent of adult BMI and genetic predisposition, which was recently published in Diabetologia. Diabetologia has marked this study as having particularly high news value for their readers.
The study found that, among the 4590 participants, lower birth weight was associated with an increased risk of developing type 2 diabetes independent of other risk factors. The data used for the study spans about 80 years, using information from birth records from as far back as 1939.
Postdoc at Steno Diabetes Center Copenhagen, Rasmus Wibaek elaborates on the findings. The initiator of the study was Professor Allan Vaag, Steno Diabetes Center Copenhagen and Lund University, Malmö, Sweden.
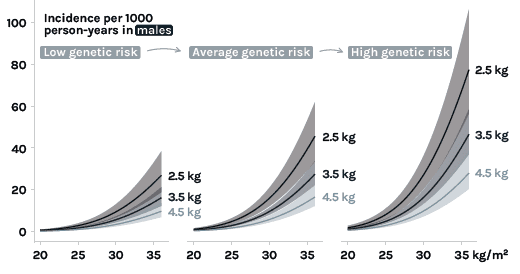
Rasmus Wibaek: Type 2 diabetes incidence rate increased with age, and the absolute rate of increase was markedly higher in persons born with lower birth weight compared with higher birth weight in a dose-response manner. Adjustment for adult adiposity (BMI) and common genetic risk influencing type 2 diabetes did not attenuate any of the associations, and the results suggested that birth weight, genetic predisposition, and BMI all are independent and strong risk factors for type 2 diabetes.

Rasmus Wibaek: Previous studies have found both inverse and u-shaped relationships between birth weight and type 2 diabetes risk. We see a clear inverse association. Unlike previous studies, we use incidence data, which, epidemiologically speaking, is a higher-ranking design for these types of associations. Moreover, we control for the genetic risk of type 2 diabetes, which previously has been proposed to explain a lot of the association between birth weight and type 2 diabetes. If we know that birth weight on its own is a strong and independent risk factor, then we would suggest that birth weight could be used as a future feasible screening criteria for type 2 diabetes, in line with genetics and family history of type 2 diabetes. As for the public health implications, it should also be noted that people with a lower birth weight, who develop overweight or obesity in adulthood are at a particularly high risk. However, as the study indicates, neither people with a lower birth weight nor those with a positive family history of type 2 diabetes, are at a particularly high absolute risk of developing type 2 diabetes, provided they keep a normal BMI throughout their lives.
Rasmus Wibaek: Although firm evidence of an association between birth weight and the risk of type 2 diabetes has been established, previous studies have been based on cross-sectional prevalence data. In this study, we were able to examine incidence of type 2 diabetes from the extensive Danish registers. Furthermore, earlier studies have not adjusted for data on common genetic risks influencing type 2 diabetes.

Rasmus Wibaek: I think our study is broadly relevant to other populations, even in populations where low birth weight is much more common than in Denmark (e.g. African and Asian populations). It can tell us something about the major challenges low- and middle-income countries will face in the coming years with a double burden of malnutrition (both high levels of low birth weight and high levels of adiposity in adults); the worst possible setup for developing type 2 diabetes and other cardiometabolic diseases. Of course, these findings need to be confirmed, but as this study took more than 80 years to make, it is the best evidence we have, and making such studies in other populations with poor data infrastructure is very hard and will take a long time. Globally, we need to act now, not in 80 years when such studies are finished.
Rasmus Wibaek: In the era of precision medicine, low birthweight holds the potential to be used as a feasible marker to guide clinical care and treatment in type 2 diabetes.
Rasmus Wibaek: Type 2 diabetes has a complex etiology with a strong contribution from adult obesity. Our findings suggest that the effects of birth weight, genetic susceptibility of type 2 diabetes, and adult obesity (BMI) are distinct and to a large extent independent risk factors for type 2 diabetes. Notably, the contribution of a lower birth weight to type 2 diabetes increases with age and may be of similar aetiological importance as the genotype.Future studies should examine how birth weight associates with other cardiometabolic outcomes, and if those who develop type 2 diabetes have a distinct cardiometabolic phenotype compared to those with a normal or high birth weight. In fact, I am already analysing these data in the cohort, and they will hopefully come out soon.
How the study was conducted
The study examined how birth weight influences age- and sex-specific trajectories of incident type 2 diabetes risk over two decades. This study included adults aged 30–60 years enrolled in the Danish Inter99 cohort in 1999–2001 (baseline examination), with information on objectively measured birthweight from original birth records from 1939–1971 and without diabetes at baseline. Birth records were linked with individual-level data on age at diabetes diagnosis. Incidence rates of type 2 diabetes by age, sex, and birth weight were estimated using Poisson modelling, adjusting for prematurity status at birth, birth order, genetic risk scores for birth weight and type 2 diabetes, maternal and paternal diabetes history, socioeconomic status, and adult body mass index (BMI).

Rasmus Wibaek: Key strengths of this study include the long-term follow-up of age-specific incidence rates of type 2 diabetes in a representative population-based Danish cohort followed for more than two decades. People with type 2 diabetes, according to the diabetes register, were excluded at baseline. As a unique dimension assessing incidence rates of type 2 diabetes, we performed OGTT at the baseline examination, allowing us to further exclude individuals with OGTT-assessed type 2 diabetes at baseline as a sensitivity analysis, and this did not change the overall findings. Further strengths include objectively measured weight at birth from original midwife records, extensive data on key covariates from both the Danish registers and the clinical examinations in the Inter99 study, as well as GWAS data in almost all participants, allowing estimations and adjustments for the currently known common genetic variation influencing birthweight and type 2 diabetes. Limitations included a lack of accurate data on gestational age among the children born at term, as well as no objectively measured data on exposure to a hyperglycaemic intrauterine environment.
The first author of the study, Rasmus Wibaek, is a postdoctoral researcher at Steno Diabetes Center Copenhagen. The study is a collaboration between Steno Diabetes Center Copenhagen, Center for Clinical Research and Prevention, and Novo Nordisk Foundation Center for Basic Metabolic Research. It is part of Rasmus Wibaek’s postdoc project, which is funded by the Danish Diabetes Academy.
12 June 2023, https://doi.org/10.1007/s00125-023-05937-0
Rasmus Wibaek, Gregers S. Andersen, Allan Linneberg, Torben Hansen, Niels Grarup, Anne Cathrine B. Thuesen, Rasmus T. Jensen, Jonathan C.K. Wells, Kasper A. Pilgaard, Charlotte Brøns, Dorte Vistiesen, Allan A. Vaag.
EAN: 5798 0022 30642
Reference: 1025 0006
CVR: 29 19 09 09